The Department of Health and Human Services Office of Inspector General recently released its 2021 Medicaid Fraud Control Units (MFCU) Fiscal Year 2021 Annual Report.
 Investigates criminal fraud
Investigates criminal fraud
Medicaid Fraud Control Units have the job of investigating criminal fraud by Medicaid providers as well as patient abuse and neglect. There are 53 MFCU offices nationally including one in each state plus the District of Columbia, Puerto Rico and the U.S. Virgin Islands. HHS-OIG oversees their activities and annually approves federal funding for these MFCU offices through a recertification process. The Medicaid Fraud Control Unit in Texas is under the Office of the Attorney General.
Only national totals provided
The 2021 annual report provides a national breakdown of criminal investigations, convictions, civil cases and civil judgments by provider type. It does not provide a breakdown by state and TDMR has requested this for Texas.
Personal care service attendants had most criminal convictions
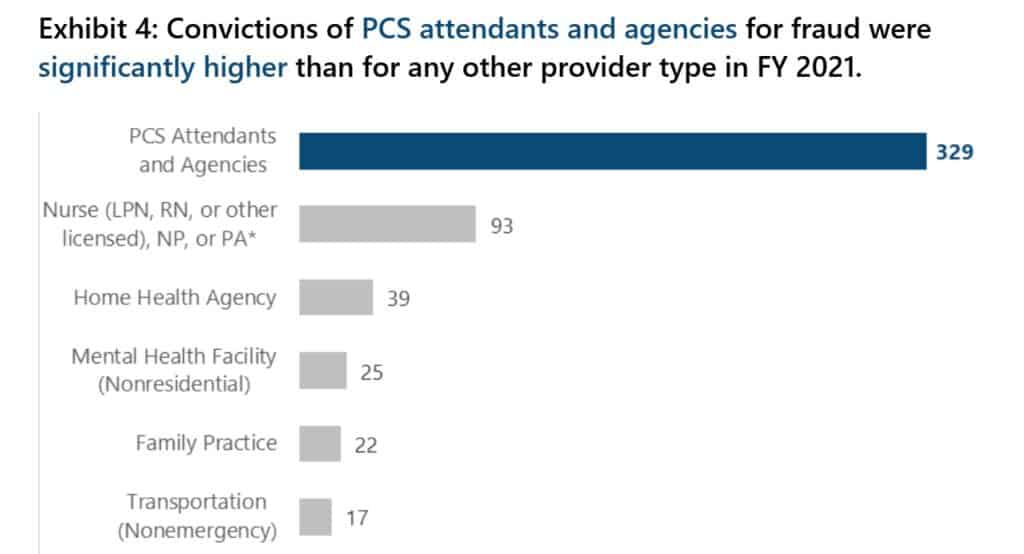
Across the country, there was a total of 780 convictions for fraud, recovering some $857 million. Personal care service attendants and agencies accounted for 329 of these with nurses ranking second with 93 convictions and Home Health Agencies with 39.
Family practice physicians accounted for 22 convictions and a recovery of $8.3 million.
Eleven dentists were found guilty of fraud resulting in a recovery of some $3.3 million. There were 10 civil judgments against dentists with a recovery of $528,864.
The results for the various provider types are shown in Appendix B of the report which is below.
More criminal investigations proportionately opened on dentists than others
However, when it came to open investigations, despite the low number of convictions and settlements, more dentists were under investigation than family practice physicians and transportation (non-emergency) in 2021. Both of these provider types ended up having higher numbers of convictions (Exhibit B2, Appendix B, p. 24 & 25).
No criminal convictions for MCO/DMOs
There were no convictions for fraud by Managed Care Organizations in 2021 despite 18 criminal investigations being opened. There were 14 civil judgments against MCOs amounting to $6.57 million.

